Introduction
Greenstick fractures are a unique type of bone injury that predominantly affects the pediatric population due to the inherent flexibility of their bones. Unlike complete fractures where the bone breaks entirely, greenstick fractures involve an incomplete break, often resembling a bent green twig. These injuries are commonly seen in long bones such as the radius, ulna, and tibia, and require prompt medical attention to ensure proper healing. At Medicover Hospitals, our team of experts specializes in diagnosing and managing greenstick fractures, offering tailored treatment options to minimize complications and promote recovery. This guide aims to provide healthcare professionals with a comprehensive understanding of greenstick fractures, from their clinical presentation to advanced treatment strategies.
What is a Greenstick Fracture?
A greenstick fracture is an incomplete fracture where the bone bends and cracks but does not completely break. This type of injury is most common in children due to the higher elasticity of their bones and the thicker pediatric periosteum, which provides additional support. The term “greenstick” originates from the analogy of a young, green tree branch that bends and splinters rather than snapping cleanly. In medical terms, this fracture occurs when the tension side of the bone fails, while the compression side remains intact.
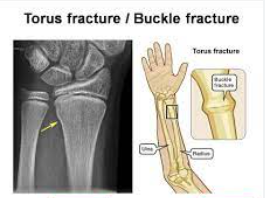
Greenstick fractures are often contrasted with other types of fractures, such as buckle fractures (torus fractures) and spiral fractures. Unlike open fractures, where the bone pierces the skin, greenstick fractures are typically closed injuries. However, they still require careful evaluation and management to prevent complications such as malunion or delayed healing. Understanding the biomechanics of this fracture type is crucial for healthcare providers to deliver effective care and ensure optimal outcomes for young patients.
Symptoms and Clinical Presentation
Children with greenstick fractures often present with localized pain, swelling, and tenderness over the affected limb. The injured area may appear deformed or bent, and the child may exhibit limited mobility or reluctance to use the extremity. In some cases, bruising may be visible, though it is less common compared to other types of fractures. A thorough physical examination is essential to assess the severity of the injury and rule out associated trauma.
Healthcare providers should also be vigilant for signs of non-accidental trauma, especially in cases where the reported mechanism of injury does not align with the clinical findings. Greenstick fractures can sometimes be subtle, and symptoms may be mistaken for sprains or soft tissue injuries. Therefore, a high index of suspicion and a detailed history are critical for accurate diagnosis. Imaging studies, particularly X-rays, play a pivotal role in confirming the diagnosis and guiding treatment decisions.
Causes and Risk Factors of Greenstick Fractures
Anatomy of a Greenstick Fracture
Greenstick fractures occur due to the unique properties of pediatric bones, which are more pliable and less brittle than adult bones. The pediatric periosteum, a dense layer of connective tissue surrounding the bone, provides additional flexibility and support. When mechanical stress is applied, the bone bends and cracks on the tension side while remaining intact on the compression side. This results in an incomplete fracture that is characteristic of greenstick injuries.
The long bones of children are particularly susceptible to this type of fracture due to their rapid growth and higher collagen content. The thicker periosteum not only contributes to the bone’s flexibility but also aids in the healing process by providing a scaffold for new bone formation. Understanding these anatomical differences is essential for healthcare providers to appreciate why children are more prone to greenstick fractures compared to adults.
Why Children Are More Susceptible
Children are at a higher risk of greenstick fractures due to the unique composition and structure of their bones. Pediatric bones have a higher water content and lower mineral density, making them more flexible and less likely to break completely under stress. Additionally, the growth plates (epiphyseal plates) in children’s bones are areas of active bone growth, which can influence the pattern and severity of fractures.
The thicker periosteum in children also plays a protective role, allowing the bone to bend rather than snap. However, this same flexibility can lead to incomplete fractures when excessive force is applied. Activities that involve high-impact or repetitive stress, such as sports or playground accidents, are common scenarios where greenstick fractures occur. Healthcare providers must educate parents and caregivers about the importance of supervision and injury prevention to reduce the risk of such injuries.
Common Causes of Greenstick Fractures
Trauma and Accidents
Trauma is the leading cause of greenstick fractures, with falls being the most common mechanism of injury. Children are naturally active and curious, often engaging in activities that put them at risk of falls from heights, such as climbing trees or playground equipment. Automobile accidents and workplace injuries (in older children) can also result in significant trauma leading to greenstick fractures.
In cases of high-energy trauma, healthcare providers should conduct a thorough assessment to rule out associated injuries, such as head trauma or internal organ damage. Prompt medical attention is crucial to ensure proper management and prevent complications. Medicover Hospitals is equipped with state-of-the-art facilities to handle such emergencies, providing comprehensive care for pediatric patients with greenstick fractures.
Sports-Related Injuries
Sports and recreational activities are another common cause of greenstick fractures, particularly in older children and adolescents. Contact sports such as football, basketball, and soccer pose a high risk due to the potential for collisions and falls. Even non-contact sports like gymnastics and skateboarding can result in fractures if a child lands awkwardly or experiences a sudden impact.
Preventive measures, such as proper protective gear and adherence to safety guidelines, can significantly reduce the risk of sports-related fractures. Healthcare providers should emphasize the importance of warm-up exercises, technique training, and supervision during sports activities. Early recognition and treatment of greenstick fractures are essential to ensure a full recovery and prevent long-term complications.
Recognizing Symptoms in Young Patients
Pain and Swelling
Pain and swelling are the most common symptoms of greenstick fractures. Children may complain of localized pain over the affected limb, which can worsen with movement or pressure. Swelling may develop rapidly, and the injured area may feel warm to the touch. In some cases, the child may guard the injured extremity, refusing to use it or bear weight.
Healthcare providers should conduct a gentle physical examination to assess the extent of the injury. Palpation of the affected area may reveal tenderness or deformity, though these findings can be subtle in incomplete fractures. A detailed history, including the mechanism of injury and the onset of symptoms, is crucial for accurate diagnosis and appropriate management.
Limited Mobility
Limited mobility is another hallmark symptom of greenstick fractures. Children may exhibit a reluctance to move the affected limb or may favor the uninjured side. In upper extremity fractures, the child may refuse to use the arm for activities such as writing or eating. In lower extremity fractures, the child may limp or avoid walking altogether.
Healthcare providers should assess the range of motion and strength of the affected limb during the physical examination. Any signs of neurovascular compromise, such as numbness, tingling, or pallor, should be promptly addressed. Early intervention is key to preventing complications and ensuring proper healing of the fracture.
Imaging Techniques for Diagnosis
X-rays: The Gold Standard
X-rays are the gold standard for diagnosing greenstick fractures. They provide detailed images of the bone, allowing healthcare providers to assess the extent and alignment of the fracture. In most cases, two views (anteroposterior and lateral) are sufficient to confirm the diagnosis. However, additional views may be necessary for complex or subtle fractures.
X-rays also help differentiate greenstick fractures from other types of fractures, such as buckle fractures or complete fractures. The characteristic appearance of an incomplete fracture with bending of the bone is pathognomonic for greenstick injuries. At Medicover Hospitals, our radiology team utilizes advanced imaging technology to ensure accurate and timely diagnosis.
When to Use MRI or CT Scans
While X-rays are typically sufficient for diagnosing greenstick fractures, advanced imaging techniques such as MRI or CT scans may be necessary in certain cases. MRI is particularly useful for evaluating soft tissue injuries or assessing the integrity of the growth plates. CT scans provide three-dimensional images of the bone, which can be helpful for complex fractures or preoperative planning.
Healthcare providers should consider advanced imaging when the clinical findings are inconsistent with the X-ray results or when there is a suspicion of associated injuries. Early and accurate diagnosis is essential for guiding treatment decisions and ensuring optimal outcomes for young patients.
Non-Surgical Treatment Approaches
Casting and Splinting
Casting and splinting are the mainstays of non-surgical treatment for greenstick fractures. These methods immobilize the affected limb, allowing the bone to heal in the correct alignment. A well-fitted cast or splint also helps reduce pain and swelling by stabilizing the injured area. The choice between a cast and a splint depends on the location and severity of the fracture.
Healthcare providers should monitor the child regularly to ensure proper healing and adjust the cast or splint as needed. Parents and caregivers should be educated on cast care and signs of complications, such as increased pain, swelling, or skin irritation. With appropriate management, most greenstick fractures heal within a few weeks without long-term consequences.
Pain Management Strategies
Effective pain management is an integral part of treating greenstick fractures. Over-the-counter analgesics, such as acetaminophen or ibuprofen, are typically sufficient to alleviate pain and inflammation. Healthcare providers should provide clear instructions on dosage and frequency to ensure safe and effective pain relief.
Non-pharmacological interventions, such as elevation and ice application, can also help reduce swelling and discomfort. Parents and caregivers should be advised to monitor the child’s pain levels and seek medical advice if the pain persists or worsens. Adequate pain control not only improves the child’s comfort but also facilitates compliance with immobilization and rehabilitation.
Surgical Interventions for Severe Cases
When Surgery is Necessary
Surgery is rarely required for greenstick fractures but may be necessary in severe cases where the fracture is significantly displaced or involves the growth plates. Surgical intervention aims to realign the bone fragments and stabilize the fracture using pins, screws, or plates. This approach is particularly important for preventing complications such as malunion or growth disturbances.
Healthcare providers should carefully evaluate the need for surgery based on the fracture’s location, severity, and the child’s age. Preoperative planning, including advanced imaging and consultation with a pediatric orthopedic surgeon, is essential for achieving optimal outcomes. At Medicover Hospitals, our multidisciplinary team ensures that surgical interventions are performed with precision and care.
Post-Surgical Care
Post-surgical care is critical for ensuring proper healing and recovery after surgery for greenstick fractures. The child may require a cast or splint to immobilize the affected limb, and regular follow-up visits are necessary to monitor progress. Physical therapy may be recommended to restore strength and mobility once the fracture has healed.
Parents and caregivers should be educated on wound care, signs of infection, and activity restrictions during the recovery period. Adherence to the prescribed rehabilitation plan is essential for achieving the best possible outcome. With proper care and follow-up, most children recover fully and resume their normal activities without long-term complications.
FAQs
Q. What is the difference between a greenstick fracture and a buckle fracture?
A. A greenstick fracture involves bending and cracking of the bone, while a buckle fracture (torus fracture) results from compression of the bone, causing it to bulge or buckle. Both are incomplete fractures common in children but differ in their mechanism and appearance on imaging.
Q. How long does it take for a greenstick fracture to heal?
A. Most greenstick fractures heal within 4 to 6 weeks with proper immobilization and care. However, the healing time may vary depending on the fracture’s location, severity, and the child’s age. Regular follow-up with a healthcare provider is essential to monitor progress.
Q. Can adults get greenstick fractures?
A. While greenstick fractures are most common in children due to the flexibility of their bones, they can occur in adults with certain conditions that weaken the bones, such as osteoporosis. However, complete fractures are more typical in adults due to the brittleness of their bones.